Osteoarthritis vs. Rheumatoid Arthritis: Understanding the Key Differences, Symptoms, and Treatment Approaches
Arthritis is a common condition that affects millions of people worldwide. However, not all arthritis is the same. The two most common types, osteoarthritis (OA) and rheumatoid arthritis (RA), are often confused due to some overlapping symptoms, but they are distinctly different in terms of causes, progression, and treatment. In this blog post, we’ll explore the fundamental differences and similarities between OA and RA, how to identify which condition you may have, and the most effective evidence-based treatment approaches for both.
What is Osteoarthritis?
Osteoarthritis (OA) is the most common type of arthritis and is often referred to as "wear-and-tear" arthritis. It is a degenerative joint disease that primarily affects the cartilage, which is the cushion-like material that covers the ends of the bones in a joint. As OA progresses, the cartilage breaks down, causing the bones to rub together, leading to pain, stiffness, swelling, and decreased joint mobility.
Key Characteristics of OA:
Progressive cartilage breakdown: The cartilage that cushions the joints wears down, leading to bone-on-bone contact.
Localized: OA typically affects one or a few joints, usually the weight-bearing ones, such as the knees, hips, spine, and hands.
Degenerative: OA develops slowly over time, with symptoms becoming more severe as the condition progresses.
Common Risk Factors for OA:
Age: OA is most commonly diagnosed in older adults, typically over 50 years of age.
Joint injury: Previous injuries, such as fractures or surgeries, can increase the likelihood of developing OA.
Obesity: Extra weight places additional stress on weight-bearing joints, increasing the risk of OA.
Genetics: A family history of OA may increase the likelihood of developing the condition.
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system mistakenly attacks the synovium, the lining of the joints. This causes inflammation in the affected joints, which can lead to joint damage, pain, and deformities. Unlike OA, which is generally localized, RA is a systemic condition that can affect multiple joints throughout the body and may also involve other organs.
Key Characteristics of RA:
Autoimmune origin: RA occurs when the immune system attacks the synovium, causing inflammation, pain, and swelling in the joints.
Symmetrical: RA typically affects joints on both sides of the body, such as both knees, both wrists, or both hands.
Systemic: RA can also affect other organs, including the skin, lungs, heart, and eyes, leading to additional complications.
Common Risk Factors for RA:
Age: RA can affect individuals at any age but is most commonly diagnosed between the ages of 30 and 60.
Gender: Women are more likely than men to develop RA, with about 70% of those affected being female.
Family history: Like OA, a family history of RA can increase the risk of developing the condition.
Environmental factors: Smoking and infections are considered triggers for RA in genetically predisposed individuals.
Similarities Between OA and RA
While OA and RA are different conditions, they share some common features, including:
Joint pain and stiffness: Both OA and RA lead to pain and stiffness in the affected joints, which can worsen with movement and improve with rest.
Swelling and inflammation: Swelling can occur in both conditions, though it’s generally more pronounced and persistent in RA.
Decreased function: Both conditions can limit movement and decrease the range of motion, making daily activities difficult.
Impact on quality of life: Both OA and RA can significantly impact a person's ability to perform activities of daily living (ADLs), such as walking, climbing stairs, or gripping objects.
However, the causes, mechanisms, and overall progression of the two conditions differ significantly.
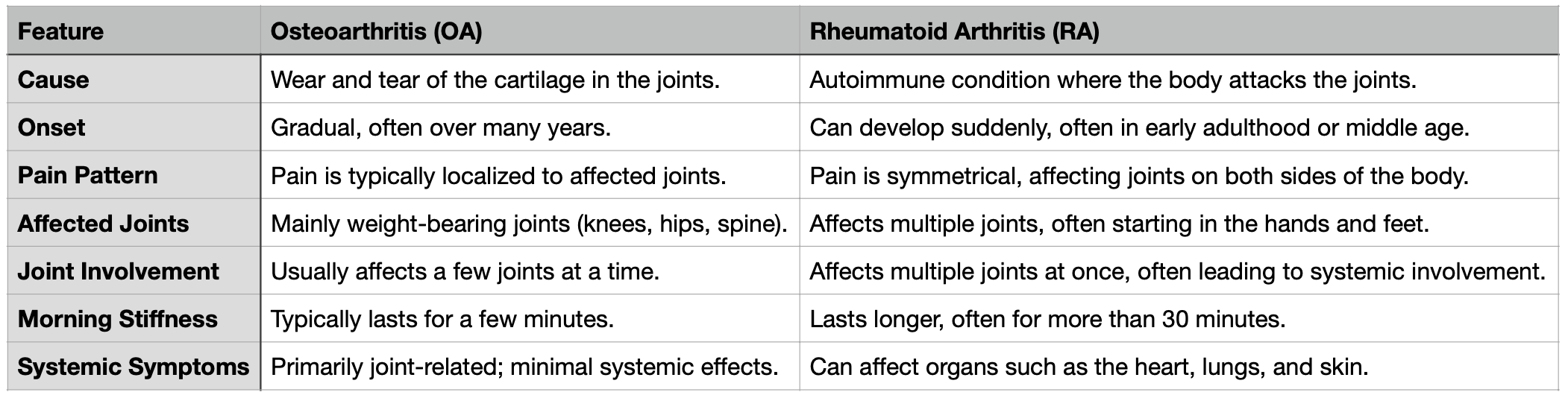
Key Differences Between OA and RA
Treatment Approaches for OA and RA
Though both conditions affect the joints, the treatment approaches for OA and RA differ, primarily due to their different causes and mechanisms.
Treatment for Osteoarthritis
The goal of OA treatment is to reduce pain, improve joint function, and slow the progression of the disease. Common treatments include:
Physical Therapy: PT focuses on strengthening the muscles around the affected joints to improve stability and reduce pain. Exercises may also help maintain flexibility and range of motion. Manual therapy and modalities like heat or cold can also provide temporary relief.
Medications: Over-the-counter pain relievers, such as acetaminophen or NSAIDs (ibuprofen), can help manage pain and inflammation. In severe cases, corticosteroid injections into the affected joints may provide temporary relief.
Lifestyle Modifications: Maintaining a healthy weight is essential for managing OA, especially in weight-bearing joints like the knees and hips. Regular low-impact exercise (e.g., swimming or cycling) can also help maintain mobility without exacerbating pain.
Surgical Options: In advanced cases where joint damage is significant, surgical options such as joint replacement or arthroscopy may be considered.
Treatment for Rheumatoid Arthritis
RA requires a more aggressive and systemic approach to treatment, as it involves chronic inflammation and can affect organs beyond the joints. Key treatments include:
Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These medications, such as methotrexate, aim to slow the progression of RA by suppressing the immune system. Biologic DMARDs, such as TNF inhibitors (e.g., Humira, Enbrel), are often used for more severe cases.
NSAIDs and Corticosteroids: NSAIDs are used to reduce inflammation and pain, while corticosteroids (such as prednisone) may be prescribed for flare-ups to control inflammation.
Physical Therapy: PT for RA focuses on improving joint function, mobility, and strength, particularly when inflammation is under control. Joint protection techniques, stretching, and strength-building exercises are used to prevent deformity and improve ADL performance.
Surgical Options: If joint damage is severe and medications are not effective, surgical options such as joint replacement or synovectomy (removal of inflamed tissue) may be considered.
Lifestyle Modifications: While exercise is important for RA, it should be performed gently and under the supervision of a physical therapist. Balancing rest and activity is key to managing flare-ups.
Conclusion
Although osteoarthritis and rheumatoid arthritis share some similar symptoms, they are two distinct conditions with different causes, mechanisms, and treatment approaches. OA is primarily a degenerative condition caused by the wear and tear of the joints, while RA is an autoimmune disorder that involves systemic inflammation. Identifying which type of arthritis a person has is crucial for determining the most effective treatment plan.
If you're experiencing joint pain or stiffness and are unsure whether it's OA or RA, consulting a healthcare professional for a proper diagnosis is essential. Early intervention, whether through physical therapy, medication, or lifestyle changes, can significantly improve your quality of life and help manage the symptoms of either condition.
At Wildflower Physical Therapy & Wellness, we specialize in treating arthritis and other musculoskeletal conditions with personalized, evidence-based approaches. Contact us today to schedule an appointment and start your journey toward better joint health and improved mobility.
If you are struggling with illness or injury and would like to get your body moving, schedule a physical therapy appointment with us today! At Wildflower Physical Therapy & Wellness, we can help you to get back to the life you want to live through pain management strategies, activity promotion and exercise. Our Cash Based Physical Therapy model allows us to deliver a highly individualized treatment plan without the fuss of insurance companies. Interested in trying dry needling to support your exercise routine and maximize recovery? Reach out to us today!